Where to find support
Find out which services may be available to you. Even if you don’t need them now, they may be useful in the future. By using the services that you are entitled to you can ensure that those closest to you don’t have to take on all the responsibility for helping you.
Find out what services can be arranged through your doctor or consultant. Living Well advisors or social prescribers may also be able to help you get support.
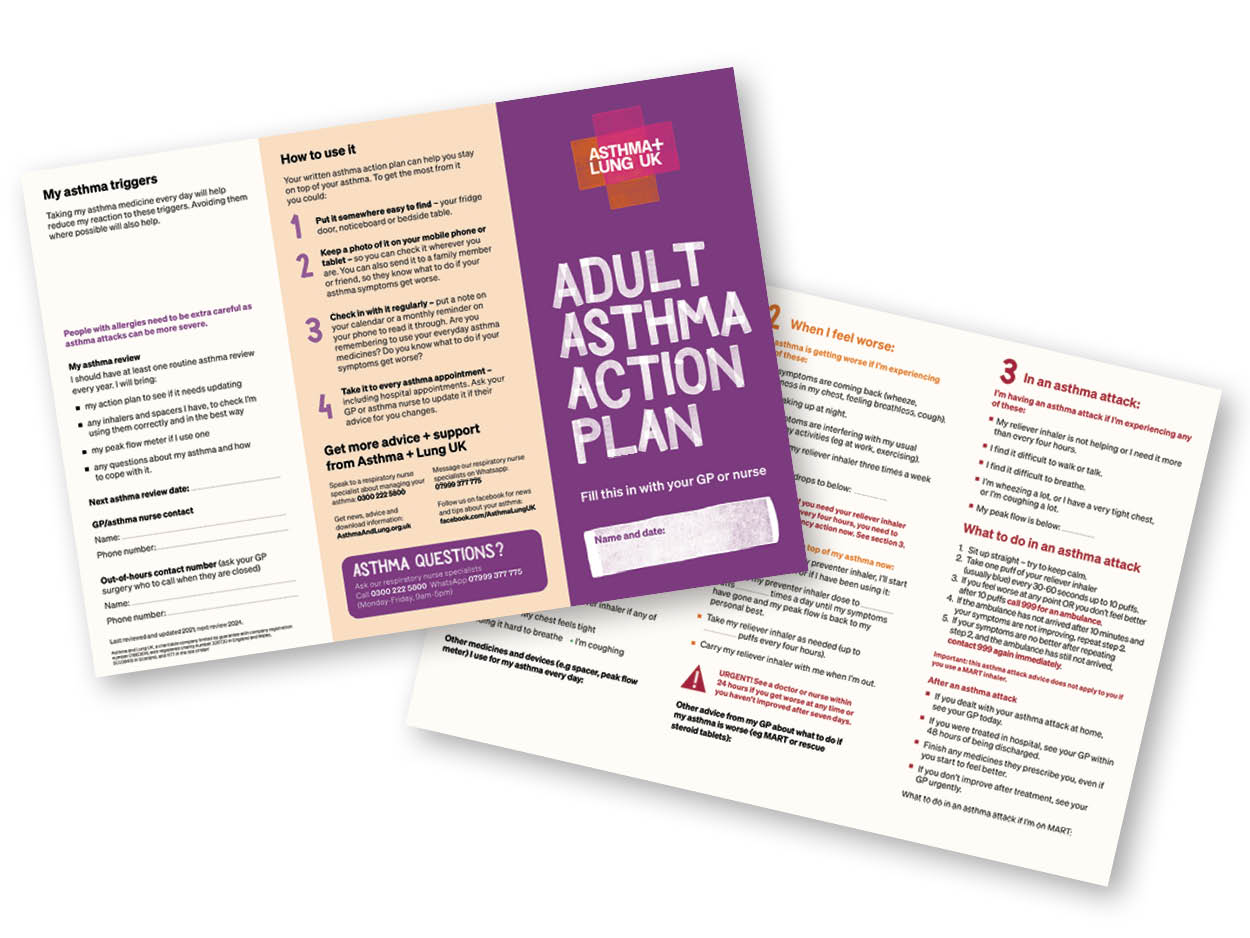
Asthma and Lung UK
You can find detailed information about asthma, its causes and how you can keep it under control on the Asthma and Lung UK website or call the helpline on: 0300 222 5800.
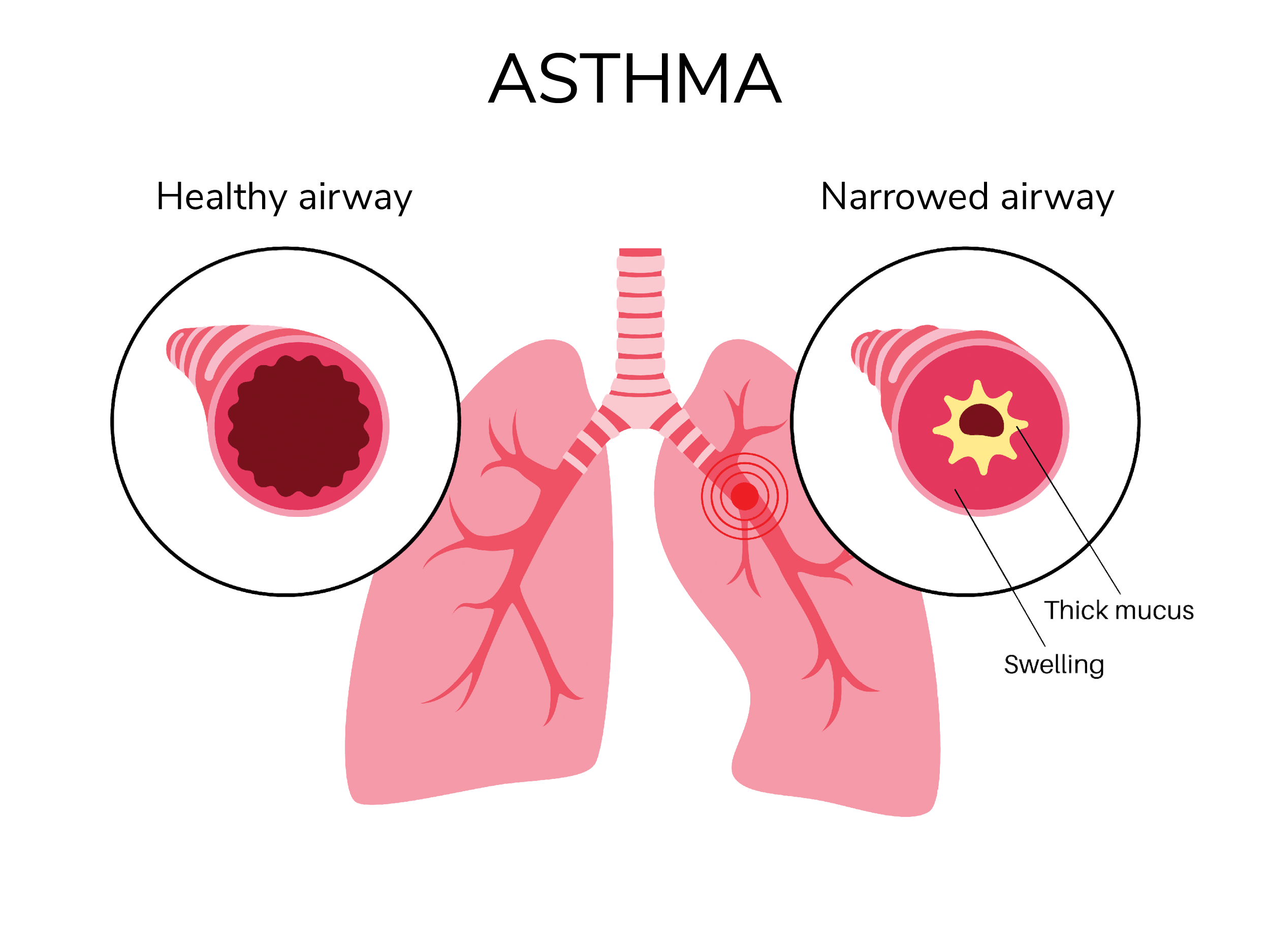
NHS Website – Asthma
You can find lots of information about the causes of asthma, diagnosis and treatment on the NHS website.
Healthy Minds
Your first step to mental health support in Bradford district and Craven
NHS Choices
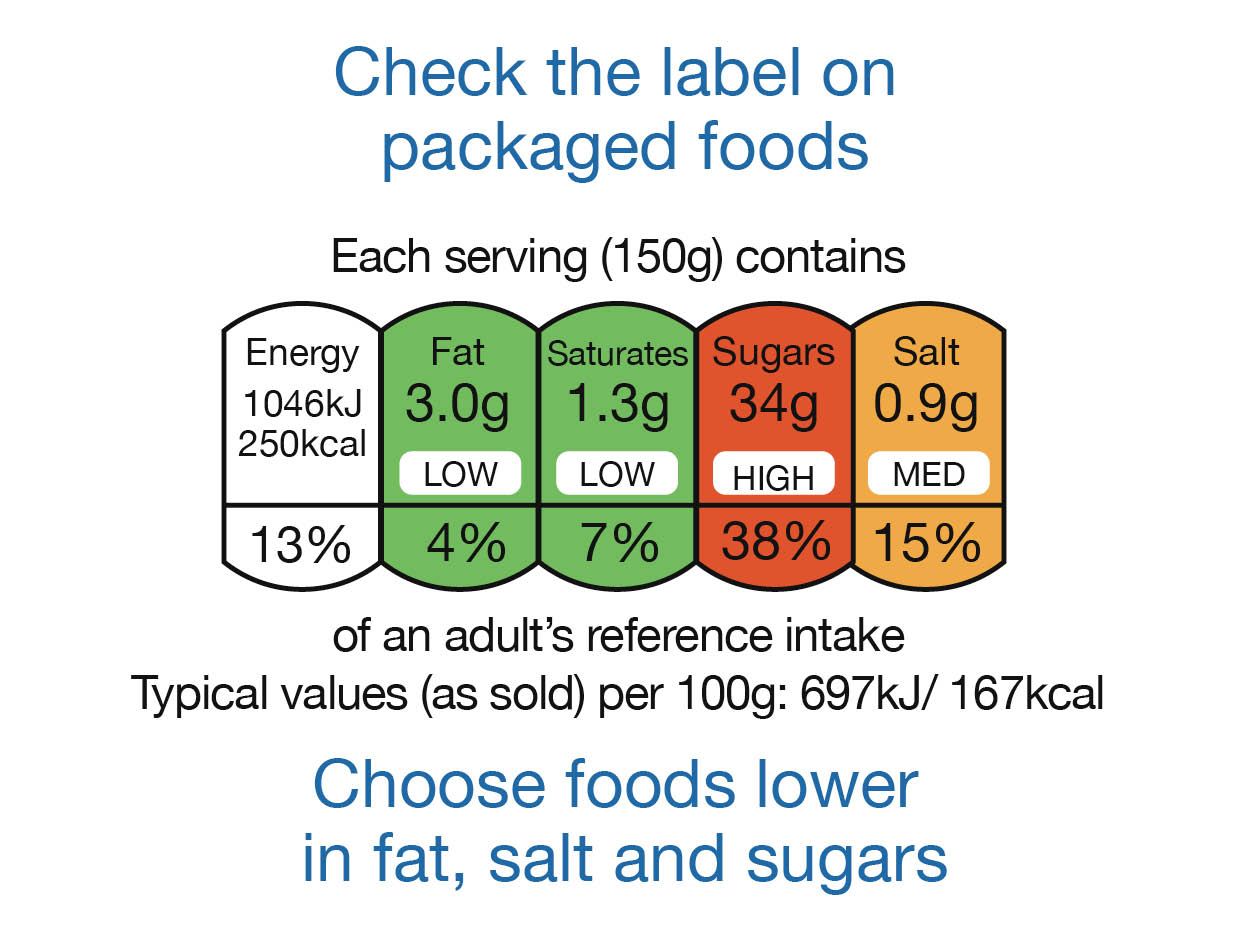
NHS advice about healthy living, including eating a balanced diet, healthy weight, exercise, quitting smoking and drinking less alcohol.
Citizens Advice Bureau
Find benefits advice or call 0844 245 1282
Bradford Council Welfare Advice
Benefits and welfare advice and help
Jobcentre plus
Find out about a benefits check with the Jobcentre Plus
Benefit calculators
Find out about independent benefit calculators
Living Well Quick Links:
Living Well Advisor Service
Free, friendly advice and non-judgemental support for anyone needing a little extra help to start making lifestyle changes. Where to start, what to do next, and signposting to other useful resources and services.
Weight Management Support
12 weeks free access to weight management groups including Slimming World, APNA Healthy Living and The Brotherhood supporting people to lose weight in a healthy way. (New members only. Offers subject to change).
Stop Smoking Service
Free confidential 1:1 support to motivate people to quit smoking with a wide range of options to help combat cravings, including free 12 week vaping kits and prescribed NRT medications.
BEEP Exercise Referral Service
A free physical activity referral service encouraging people who are inactive, to become more active with a 52 week support programme. Also a great option for people living with a long term health condition.